Office of Clinical Quality Management
OCQM Vision: To build a culture of continuous assessment of quality, drive systemic data-driven decision-making, and improve support services provided by OCQM across the DBHDS service system
OCQM Mission: To equip our partners, across the DBHDS service system, with the tools, resources, training and consultation necessary to identify systemic opportunities for: 1) quality improvement; 2) risk reduction; and 3) quality assurance; ultimately resulting in positive impacts on individuals and families served.
The Office of Clinical Quality Management (OCQM) supports the development and expansion of an agency-wide quality management plan by ensuring high quality service delivery focused on:
- prevention,
- early intervention,
- effective treatment, and
- recovery and rehabilitation.
The office works with interdisciplinary teams to achieve system-wide community inclusion, safety and well-being, recovery and self-empowerment outcomes (related to behavioral health and developmental service provision) across all service setting areas, including community and hospital based care.
The office facilitates inter-departmental, inter-agency, and cross-sectoral alignment of quality improvement initiatives for DBHDS. OCQM provides oversight of quality improvement efforts and responds to trends, by ensuring quality improvement initiatives are developed and corrective actions and regulatory reforms are implemented, if necessary, to address weaknesses/service gaps in the system.
The office staff supports the Quality Improvement Committee (QIC) structure, which oversees the work of the Developmental Disability quality committees. In addition, the office partners with and facilitates efforts within DBHDS divisions to ensure that quality improvement activities, including best practices and evidence-based outcomes, are coordinated and integrated into the primary functions of the organization. OCQM oversees and directs contractors who perform community-based quality review processes for DBHDS including the Quality Services Reviews and National Core Indicators.
The Office of Community Quality Management oversees the Office of Community Quality Improvement
Community Behavioral Health Quality Management is focused on enhancing the quality of behavioral health care through the design, implementation, and evaluation of the Behavioral Health Quality Management System (BH QMS)
QM System Goal:
A system of quality services that allows individuals to direct their own lives and recovery, to access and fully participate in their community and balance risk, health, safety and well-being.
The Division of Clinical & Quality Management oversees the quality management system (QMS), which is based on DBHDS’ vision, mission, and strategic plan. A multi-faceted approach inclusive of nationally recognized quality principles and frameworks is the foundation for DBHDS’ culture of quality and its quality infrastructure. An effective framework includes quality assurance, risk management, and quality improvement processes.
Quality Assurance focuses on discovery activities to test compliance with standards, regulations, policies, guidance, contracts, procedures and protocols, and the remediation of individual findings of non-compliance.
Risk Management assess and identifies the probability and potential consequences of adverse events and develops strategies to prevent and substantially mitigate these events or minimize the effects.
Quality Improvement is the systematic approach aimed toward achieving higher levels of performance and outcomes through establishing high quality benchmarks, utilizing data to monitor trends and outcomes and resolving identified problems and barriers to goal attainment, which occurs in a continuous feedback loop to inform the system of care.
This graph shows the quality framework employed by the DBHDS QMS. 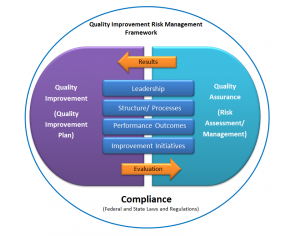
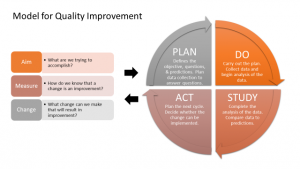
The DBHDS Quality Management program utilizes the Plan-Do-Study-Act quality improvement model depicted below. (Source: Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance (2nd edition). San Francisco: Jossey-Bass Publishers; 2009. )
DBHDS’ quality committees assist the quality management system (QMS) through the performance of critical tasks related to data review and analysis, establishment and monitoring of performance measure indicators (PMIs), and the implementation of approved quality improvement initiatives (QIIs). DBHDS’ committee structure is shown here:
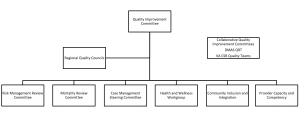
Quality Improvement Committee (QIC) – the highest level quality committee for the agency and provides overall oversight of the quality management program. All other quality committees report to the QIC. The QIC ensures a process of continuous quality improvement and maintains responsibility for prioritization of needs and work areas and resource allocation to achieve intended outcomes for the agency and Commonwealth.
Regional Quality Councils (RQCs) – a regional quality committee under the QIC, the RQCs include individuals with disabilities, a family member, providers and DBHDS staff. The RQCs review and analyze state and regional data, identify trends, provide input to the QIC and make recommendations for systemic improvement including recommending quality improvement initiatives for implementation in response to identified areas for improvement. There are five RQCs, one per DBHDS region.
Risk Management Review Committee (RMRC) – this quality committee seeks to improve quality and safety by learning from past performance, errors and near misses, and to gain awareness of areas of vulnerability in practice and to improve these areas, thereby creating a safer environment for the delivery of services. The RMRC establishes goals and performance measure indicators, along with quality improvement initiatives, that affect outcomes related to safety and freedom from harm and avoiding crises.
Mortality Review Committee (MRC) – this quality committee reviews and collects mortality data for individuals with intellectual and development disabilities who received services from a DBDHS licensed provider at the time of death. The MRC’s purpose is to identify and implement system-wide quality improvement initiatives to reduce the mortality rates for this population to the fullest extent practicable.
Case Management Steering Committee (CMSC) – this quality committee is responsible for monitoring case management performance across responsible entities to determine progress toward meeting established Support Coordinator/Case Management targets. Based on this data review and system analysis, the CMSC recommends systemic quality improvement initiatives to the QIC, provides technical assistance, and makes recommendations for action under the Performance Contract when targets are not met.
KPA Workgroups – collectively, the Health, Safety and Wellbeing, Community Inclusion and Integration and Provider Capacity & Competency workgroups are known as the KPA Workgroups. The KPA Workgroups analyze data directed at helping individuals achieve positive outcomes, promote service provisions in the most integrated settings and ensure full access and participation in community life, and improving availability of and access to DBHDS services across the Commonwealth and facilitate provider training, competency and quality service provision. They establish goals and performance measure indicators along with recommending quality improvement initiatives specific to each individual workgroup.
Quality Collaboratives – these collaboratives provide opportunities for enhanced collaboration and coordination of quality at a cross-agency or cross-sectoral level. The aim is to align shared missions and visions and provide a forum to enhance communication and data sharing through a single process. The collaboratives may inform the QIC but are not considered to be a sub-committee of the DBHDS QIC.
What is the National Core Indicators Project?
The National Core Indicators (NCI) Project is a collaboration between the National Association of State Directors of Developmental Disabilities Services (NASDDDS), the Human Services Research Institute (HRSI) and voluntary state participants, including Virginia. The core indicators are standard measures used across states to learn about the outcomes of supports and services provided to individuals and families and to establish national benchmarks. These indicators provide an overall view of system performance, assess performance in NCI established domains and subdomains. NCI partners use the data and reports to achieve goals including:
- Enhance practice at the state level
- Influence public policy
- Inform strategic planning
- Contribute to the scientific literature
While NCI has two initiatives focused on intellectual and developmental disabilities (IDD) and aging and disabilities (AD), DBHDS currently participates only in the NCI-IDD initiative.
NCI groups the indicators into these domains:
- Individual outcomes
- System Performance
- Health, Wellness and Rights
- Family Experience
NCI surveys include the
- In-Person
- Adult Family
- Family Guardian
- Child Family
- State of the Workforce
To learn more about NCI, the surveys and data briefs and highlights, please visit https://nationalcoreindicators.org.
How is DBHDS involved with NCI?
DBHDS contracts with VCU Partnership for People with Disabilities to fulfill the requirements for participation in the NCI Project IDD initiative. To learn more about the NCI IDD Project, please visit: https://nci.partnership.vcu.edu/nci—idd-project/ .
As the NCI Project focuses on engaging those served and those who serve through surveys, participating in the surveys gives individuals, their families, and those who provide the services and supports the opportunity for their voices to be heard directly.
We believe that the voices of people who receive public services and their families should be heard directly. No one should be preemptively deemed “unable to respond”. (National Core Indicators)
Commencement of NCI Survey Year
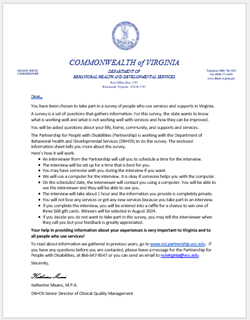
The 2023-2024 NCI In-Person Survey is underway. Each year, the Partnership randomly selects individuals (and their families) to participate in the surveys, which include an interview. For individuals and families selected, a letter is sent that outlines what to expect while participating in the survey and includes information about the survey. The letter looks like this:
The 2023-2024 NCI Adult Family and Family Guardian Surveys are underway. Selected participants receive the survey. The cover letters look like this:

Here’s how you can help:
If you’re an individual, you can choose to participate in the survey.
If you’re a family member, you can choose to participate in the survey and/or help your family member participate.
If you’re a legal guardian, you can choose to participate in the survey and/or help individuals participate.
If you’re a provider, you can support the individual/family/guardian in participating in the survey and respond to calls and emails from interviewers.
To find out other ways in which you can help, please visit Frequently Asked Questions.
To learn more about the NCI IDD Project, please visit: https://nci.partnership.vcu.edu/nci—idd-project/
You can also contact VCU Partnership for People with Disabilities:
- Leave a message at 866-647-8547
- Send an email to: ncivirginia@vcu.edu
- VCU Virginia’s National Core Indicators Project Reports
- National Core Indicators website (VCU website)
- DBHDS Developmental Disability QM Plan (Part I, II, III) SFY2021
- DBHDS Developmental Disability QM Plan (Part I & II) SFY2022
- DBHDS Developmental Disability QM Plan (Part I & II) SFY2023
- DBHDS Developmental Disabilities QM Plan (Part I & II) SFY2024
- DBHDS Developmental Disability QM Plan Annual Report
- DBHDS Developmental Disability QM Annual Report and Evaluation SFY2023
Looking for information on QI training and resources? Please visit Clinical and Quality Management QI Library.






